Appointment Timing - 9am to 6pm
What’s Wrong With My Gallbladder?
Gallstones
This is a patient information booklet providing specific practical information about gallstone disease in brief. Its aim is to provide the patient & his or her family with useful information on this particular gallbladder problem, the procedures and tests you may need to undergo, treatment approaches, risks involved, duration, expenses and helpful advice on coping successfully with the problem. If you require more information, Dr. D.R.Kulkarni or your doctor will be able to provide more information.
Gallstones / Gallbladder Stone: Symptoms, Causes and Treatment Options
Click Here For Quick Links of Article
- What Is Gallbladder?
- Function Of Gall Bladder?
- Is Gall Bladder Necessary For Survival
- What Are Gallstones?
- Types Of Stones
- How Do Gallstones Form?
- Who Gets Gallstones?
- Do Gall Stones Always Cause Symptoms?
- What Problems May Gallstones Cause?
- Can Gall Stones Cause Cancer?
- What Is Biliary Colic?
- Are There Unusual Presentations?
- What Tests Might I Have?
- Treatment For Gallstones
- Can Only Removal Of Stones Suffice?
- Can Gall Stones Be Fragmented & Removed Like Kidney Stones (ESWL)?
- Can Gallstones Be Dissolved?
- Role Of Alternative Treatments?
- What Happens If I Don’t Want Surgery Immediately?
- Do I Need To Be On A Special Diet?
- When Is Cholecystectomy Advised For Gall Stones?
- What Is Laparoscopy?
- How Do I Prepare For Surgery?
- What Anaesthetic Will I Have?
- How Is Laparoscopic Cholecystectomy Performed?
- What May Necessitate Conversion To Open Surgery?
- What Will Happen After Surgery?
- What Are The Benefits Of Keyhole Surgery?
- Who Can’t Have The Procedure?
- What Are The Problems Of Open Surgery?
- Will I Suffer A Lot After Surgery?
- What Are The Possible Risks And Complications?
- Do I Need To Diet Afterwards?
- When Do I Resume Activities?
- Will I Be Called Back To Hospital?
- When Should I Call My Doctor After Surgery?
- Can People Manage Without A Gall Bladder?
What Is Gallbladder?
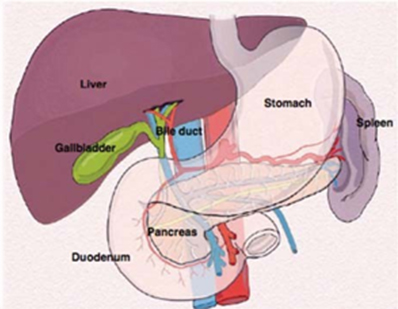
Gall is an old-fashioned word for what we now call bile. The gallbladder is a small sac that lies beneath the liver in the right upper abdomen under the rib cage. It is joined to the bile duct, a tube that comes from the liver and carries bile to the intestine. Bile is a yellow-green viscous fluid helpful in digesting food is produced in liver.
What Is The Function Of Gall Bladder?
The gallbladder stores bile that is produced by the liver and removes water and salt from it. It contracts when we eat, especially fatty food and pushes bile down the bile duct into the intestine.
Is Gall Bladder Necessary For Survival / Digestion / Good Health
The gallbladder is not necessary to maintain good health. After the gallbladder is removed, bile duct increases in diameter slightly and bile flows directly from the liver to the intestines, and digestion proceeds normally.
What Are Gallstones?
Gallstones are solid pieces of stone-like debris formed from bile, usually in the gallbladder and then pass off into the bile duct. But they can uncommonly form in the bile duct. Stones are not passed from the bile duct to the gall bladder.
What Are The Various Types Of Stones?
The commonest type consist of cholesterol. They are pale in color. Others are made of calcium bilirubinate, are dark in color and are called pigment stones. Some patients have mixed stones.
How Do Gallstones Form?
Gallstones start as tiny crystals, then grow to resemble gravel, and may end up looking like pebbles. Sometimes, there is just a single stone; often there are several and it is not unknown for the gallbladder to contain literally dozens of small stones.
Bile is a mixture of different chemicals. When the bile can no longer hold these chemicals in a liquid solution, chemicals start crystalizing. Gallstones most frequently contain cholesterol. You may have heard of cholesterol as a fatty substance in our diet that can cause disease in arteries.
Cholesterol may be bad for arteries but the liver finds it very useful. Bile contains lots of cholesterol and indeed it is an important way for the body to clear itself of any excess. Bile may contain so much cholesterol that when it is stored in the gall bladder the cholesterol may separate out as little crystals, which may clump together to form a gallstone.
Who Gets Gallstones?
Gallstones are very common, but most people who have them do not know. By the age of 60 nearly a quarter of women (and a rather smaller number of men) will have developed some gallstones.
The old saying that gallstones are seen in people with all the ‘Fs’ (fair, fat, female, fertile and forty) has some truth in it, since gallstones are commoner in women, especially those who have had children and who are overweight. However the age at which gallstones may give symptoms has changed a lot in recent years, and doctors see gallstones in much younger women, sometimes even teenagers, although it is certainly true to say they become commoner as we get older. They do seem to be getting rather more common generally, possibly as a result in changes in our diet over the last two generations.
Contraceptive pills & pregnancy increases risk of gall stone formation. Gallstones are also associated with a diseased gallbladder that is not functioning (contracting) properly. They are also found in patients with past history of typhoid and patients with poor thyroid gland function ( hypothyroid ). Sometimes they are formed around the eggs of roundworms who wander in the biliary tree occasionally.
Do Gall Stones Always Cause Symptoms?
Many people with gallstones have no symptoms and may never develop any problem. They can be found quite incidentally, for example, in somebody who is having ultrasound scan done for a completely different reason. Indeed doctors think that most people who get gallstones at some stage during their life are never aware that they have them. In that situation, such stones are best left alone unless they go on to cause symptoms. This only happens in a minority of patients. It is not always clear why gallstones should cause problems for one individual yet leave another quite unaware of their presence.
Gallstones gradually enlarge over years, but it is often small stones that tend to cause more symptoms and are more likely to cause complications.
What Problems May Gallstones Cause?
The consequences of gallstones can range from brief attacks of pain to potentially serious complications, such as inflammation of the gall bladder or pancreas. Gall stones usually give rise to symptoms if they move from the gall bladder into one of the tubes (known as bile ducts) that lead from the gall bladder into the intestine. If they get stuck in the narrow neck of the gall bladder or cystic duct, this can cause pain which can be quite severe. This type of pain is called biliary colic. Alternatively, the stones may cause inflammation in the wall of the gall bladder (known as cholecystitis). If a stone gets into the main duct leading from the liver into the intestine it can give rise not only to pain from biliary colic but it may block the flow of bile from the liver altogether which causes jaundice or even blockage of flow of pancreatic juice and pancreatitis.
Commonly problems of gall bladder and bile duct show up with abdominal pain especially in the right upper abdomen. Pain can be of acute nature or low grade over some time and is often accompanied by nausea, vomiting, intermittent fever, loss of appetite & jaundice. Not every patient will have all the symptoms but a combination will be present depending on at what stage of illness the patient presents. Often the disease is picked up during routine health check up.
On examination your doctor will find some sharp or dull tenderness in the abdomen, sometimes jaundice, a lump if present & palpable to the examining fingers.
Can Gall Stones Cause Cancer?
Yes. Gall stones have shown a strong association with gallbladder cancer especially in Indian subcontinental patients. Persistent inflammation of gall bladder wall by stones causes changes in the lining of gall bladder bringing about the malignant change over a long time.
What Is Biliary Colic?
By far the commonest symptom caused by gallstones is biliary colic.
Biliary colic is a pain that is felt in the top of the stomach, either in the middle or just under the ribs on the right hand side. It is usually a continuous pain but may come in waves. It is usually rather more severe than ‘indigestion’ and it is not uncommon for patients to feel so uncomfortable that they may seek medical advice. The pain usually lasts for a few hours and then goes away. Occasionally patients may feel sick or may vomit. The pain often follows a meal and may be noticed most often in the evenings – but one of the most irritating features of biliary colic is that it may occur at any time. Sometimes pain radiates to other part of body like shoulder or back especially when there is inflammation of gall bladder or pancreas or stone is in the bile duct.
Even very small gallstones can cause a lot of symptoms. Actually it is the small stones are the ones that cause more complaints and complications like jaundice or pancreatitis. A large stone usually causes problems limited to the gall bladder like inflammation( cholecystitis), infection(empyema) or gangrene since they find it difficult to slip down. A patient with cholecystitis or pancreatitis or stones in the bile duct can occasionally present in a very critical condition due to severe infection.
Are There Unusual Presentations?
Yes, occasionally patients present with severe sepsis due to stones in the gall bladder or bile duct or pancreatitis and land up in the ICU straight in a very critical condition.
What Tests Might I Have?
You would probably have some blood tests to look for signs of inflammation or jaundice. These include CBC & LFT. Amylase & lipase levels in the blood are always checked in the blood to rule out pancreatitis.
The best test for gallstones is an ultrasound scan or USG. Gallstones reflect ultrasound very well and are easily detected, unless they are sonolucent or deep in the abdomen or hidden behind some gas in the intestine. If the ultrasound scan does not give a clear result then other tests are done. Fortunately there are a number of different ways of scanning the gallbladder that enable doctors to say with confidence whether or not you have gallstones like CT scan, MRCP, ERCP or EUS.
What Is The Ideal Treatment For Gallstones?
The ideal treatment for gallstones with symptoms &/or complications is removal of the gall bladder with the stones inside (cholecystectomy). There is no adverse effect on digestion due to removal of gall bladder.
This is usually done in one of two ways. If the stones are all contained in the gall bladder, then the simplest method is to have a small operation to remove the gall bladder and the stones within it. These operations can nowadays be done with keyhole surgery also called laparoscopy which means that patients recover from the operation within just a day or two, a huge improvement from the much larger operations that used to be necessary for gallstones in the past. However conventional open surgery may still be required occasionally.
The other way of dealing with gallstones, by endoscopy, is used for stones that have found their way into the common bile duct and caused a blockage there. Such stones can often be treated with ERCP followed by cholecystectomy in next 2-3 days.
If they are not causing any symptoms however, then it may not be necessary to have any treatment at all. Even if you have a single attack of pain from gallstones, there may be no further trouble for many years, if ever.

Can Only Removal Of Stones Suffice?
In the 70’s & early 80’s exclusive stone removal was in vogue. But it was given up as the diseased gall bladder remains in the body, can reform stones & also develop cancer in the long term. Stone removal is now suggested only in patients with emergency situation where major surgery cannot be taken up
Can Gall Stones Be Fragmented & Removed Like Kidney Stones (ESWL)?
In a very small number of patients, gallstones can be broken up by using shock waves. These are usually large Stones in the gall bladder or bile duct and are broken into small pieces by an external device called lithotripsy and then extracted by endoscopic procedure.
But this procedure is not still the gold standard of therapy as it leaves behind the diseased gall bladder which can reform stones, can develop cancer. Also it is not possible to remove the stone sand or gravels to their last extent and therefore risk of pancreatitis remains and one needs to have a tube/stent in the bile duct for a long time after this, not to mention the multiple endoscopic procedures that the patient would require with their inherent risk & high cost. Hence this form therapy should be reserved for very selected patient, in selected high volume institutes and only if your surgeon suggests you to do so.
Can Gallstones Be Dissolved?
Oral bile acid preparation Ursodeoxucholic acid ( UDCA) is often prescribed. But one should realize that this drug can dissolve only cholesterol stones, very small in size & limited in number. Taking bile acids by mouth has largely gone out of vogue because treatment was lengthy, success rates were modest and recurrence of gallstones was frequent. Additionally, cost of oral bile acid therapy quite often exceeds that of surgery.
Then What Is The Role Of Alternative Treatments?
Their use is limited to patients who are not suitable for surgery or those who don’t want surgery. There are no good alternatives to surgical removal of the gallbladder.
What Happens If I Don’t Want Surgery Immediately?
If you have had episodes of pain that your doctor thinks are due to gallstones, it is likely that you will be offered surgery unless you are so unfit that an operation would be too risky. If you do not like the idea of surgery, you might choose to wait and see what happens to you. It is likely you will continue to have bouts of pain. But a small section of people with gallstones do develop other complications. A small number of people will get jaundice & will require an endoscopy for relieving it. Rarely, a gallstone can block the pancreas. This leads to a potentially serious complication called acute pancreatitis. If you are going to choose not to have surgery, do ensure that you are aware of the small risk that you are running.
Do I Need To Be On A Special Diet?
Some people find that heavy meals or particular foods, especially those, which are fatty or oily aggravate their symptoms. You may benefit by staying on a low-fat diet till the operation.
A low fat diet preferably including steamed or boiled vegetables, fruit, pasta which is oil free, steamed or poached fish or skinless chicken, grilled lean meat, skimmed milk, soya protein such as tofu, brown bread, various types of beans and pulses such as lentils is helpful.
After a gallbladder operation you can introduce fats into your meals although it is healthier to avoid them if possible. Most people can eat moderate amounts of all their favorite foods without trouble.
It is best to avoid alcohol if you have liver or gallbladder trouble. When you have recovered from a gallbladder operation, however, you should be able to drink again if you wish, within the usual limits.
When Is Cholecystectomy Advised For Gall Stones?
The gallbladder is removed when you have symptoms due to stones ( abdominal pain, nausea, vomiting, jaundice, pancreatitis) or inflammation in your gallbladder. A patient who has stone/stones in the gall bladder but has no complaints (asymptomatic) is usually not advised surgery as it has been shown that gall bladder stones may not cause complaints for long time. This is especially true for solitary large stones. But small stones behave more erratically and can cause complications and hence such patients are better served with surgery.
This operation is performed to prevent you from having further attacks of pain, or complications such as inflammation of the pancreas. If you have medical problems that make it highly risky to undergo surgery, you may be advised against having the operation or postpone the surgery till suitable time.
What Is Laparoscopy?
Laparoscopy, or "keyhole" surgery, enables the surgeon to inspect the inside of the abdomen, without having to make a large cut. A laparoscope is a long, narrow telescope attached to a small video camera and a light. It provides a view of the inside of the abdomen on a TV monitor for the surgeon and other team members.
How Do I Prepare For Surgery?
Try to stop smoking as soon as you know that you need an operation. This will reduce your chances of developing complications after surgery.
Please bring a list of all your medication with you to the hospital. You need to stop certain medications like those used to prevent clotting of blood ( heart patients / diabetics) 4 to 5 days in advance in consultation with your surgeon and regular physician. Some patients may need the surgery while on these medications or stopping the medications is contraindicated in them. At such times the added risk of postoperative bleeding should be kept in mind.
Follow the instructions provided by the nursing staff. Do not eat anything for at least 6 hours before the procedure. You may be allowed to take your usual medication with sips of water.
What Anaesthetic Will I Have?
Removal of the gallbladder requires general anaesthesia, i.e. you will be made unconscious. The anaesthetist will meet you previously and explain the procedure. A tube will be put down your windpipe while you are asleep, so you may experience a sore throat afterwards.
How Is Laparoscopic Cholecystectomy Performed?
Laparoscopic cholecystectomy is complete removal of the gallbladder by keyhole surgery, without a big cut. A small incision 2 to 3 cm long is made at the navel and the laparoscope is inserted. The surgeon inflates the abdomen with carbon dioxide, a harmless gas, to provide room for the surgery to be performed. Two small cuts 0.5 to 1 cm in size are made below the right rib margin. A fourth cut is in the upper abdomen close to the breastbone. These are used for inserting instruments, such as scissors and forceps, which can pick up and cut tissues. Surgical clips are placed on the duct and artery leading to the gallbladder in order to secure these structures against leakage or bleeding. The gallbladder is removed from inside the abdomen through one of the cuts in a specimen bag. This cut may need to be enlarged slightly if the gallstones are large.
It is sometimes necessary to take an X-ray of the bile duct during the operation. This is performed if there is some doubt that you may have a stone in the bile duct.
The surgery normally takes 30 to 90 minutes, depending on the size of the gallbladder, how inflamed it is, and the difficulty of the operation.
What May Necessitate Conversion To Open Surgery?
A severely inflamed or scarred gall bladder, difficulty in understanding the local anatomy especially of the artery and duct, bleeding, very thick gall bladder, multiple previous attacks of inflammation, adherence to surrounding vital organs like stomach or large intestine, previous abdominal operations with adhesions, doubt of a malignancy are the factors responsible for lengthy surgery & may force the surgeon to convert laparoscopic operation to a conventional open surgery in view of patient safety and to avoid complications like bile duct, hepatic artery & portal vein injury. The operation is completed through a larger incision, under the same anaesthetia. This incision is 4 to 6 inches long, beneath the ribs in the right upper abdomen. A conversion should always be looked at as a safety measure than a negative step.
What Will Happen After Surgery?
You will return to the ward after spending some time in the recovery area of the operating suite. The nurses will monitor your progress and administer painkillers. Most patients are able to get out of bed and start eating later the same day. You may be able to leave the hospital later that day or the next morning or in couple of days depending on your condition, your original pathology and the protocol of individual surgeon.
What Are The Benefits Of Keyhole Surgery?
The advantages to you of having your gallbladder removed by the laparoscopic method are:
- Reduced pain and ease of recovery after surgery
- Less pain medication required
- Shorter hospital stay
- Earlier return to full activity and work
- Less visible abdominal scars
Who Can’t Have The Procedure?
Most patients can have laparoscopic surgery, if they are able to tolerate general anaesthesia safely. A few conditions make laparoscopic surgery difficult or unsafe. In these instances, your surgeon may advise you to undergo the traditional “open” procedure. Open cholecystectomy remains a safe and effective alternative.
What Are The Problems Of Open Surgery?
The disadvantages to you of having your gallbladder removed by the open method are:
- longer recovery after surgery
- more pain medication required
- longer hospital stay
- late return to full activity and work
- more chance of wound infection & abdominal scars
Will I Suffer A Lot After Surgery?
Pain after laparoscopic surgery is usually mild to moderate. You may also feel some shoulder pain. This is due to stretch on the diaphragm and usually disappears in 2-3 days. You will be given painkillers and made comfortable. The surgeon will also put local anaesthetic into the cuts in your tummy. You will be given regular pain medication on the ward.
If you need the bigger open operation, you are likely to feel more pain afterwards. In this case, we will give you a PCA (patient- controlled analgesia), a button to press whenever you feel pain. A computerised pump will deliver a small amount of morphine from a syringe into your vein. For a few minutes after one dose, the pump will not deliver another dose, no matter how often you press the button. This will enable you to safely control the amount of painkiller that you receive.
After discharge from the hospital you are advised oral analgesics. These are mild analgesics and are stopped in 3-4 days
What Are The Possible Risks And Complications?
Laparoscopic cholecystectomy offers substantial advantages over open cholecystectomy. While the likelihood of major complications is very low, certain risks do exist. These risks may be higher in your case, if you have serious medical problems that increase the risks of general anaesthesia. Most of these risks are also present with the open method of cholecystectomy. A few complications, such as bile duct injury, may be slightly more common after laparoscopic surgery. The possible complications include:
- Those related to general anaesthesia, including the rare incidence of death
- Bleeding
- Infection
- Blood clots forming in the legs
- Leakage of bile from the bile ducts into the abdomen (about 1 in100 patients)
- Injury to the bile duct, which usually needs repair (about 1 in 200patients)
- Injury to abdominal organs (about 1 in 1000 patients)
Do I Need To Diet Afterwards?
You can have a normal diet soon after the operation. Most patients find they prefer light food and multiple small meals for a few days. There are no long term dietary restrictions advised specifically due to gallbladder removal. There is no effect on digestion.
When Do I Resume Activities?
Following laparoscopic cholecystectomy you may return to normal activities, driving and work, usually within 10 to 15 days. After 15 days you can resume exercises like brisk walking. You should avoid strenuous activities for 3 months. Swimming can be started after 3-4 months. Lifting heavy weight should be avoided for 6 months. Sexual activity can be started after 1 month. YOGA should not be performed for 1 year. All these restrictions are advised so that you do not develop a postoperative incisional hernia, which can occasionally occur especially through the umbilical wound. You can develop this hernia otherwise also if you are obese or develop obesity later, or if you develop increased intra abdominal pressure due to some other reason like constipation or straining at urine or due to persistent cough.
In case you undergo the open operation, you will need 3- 5 weeks to resume light work.
Will I Be Called Back To Hospital?
You need to come back to the hospital for a follow up visit & skin suture removal one week from surgery and otherwise if you have specific problem like fever, jaundice, severe abdominal pain, abdominal distension, vomiting etcetera.
What Is Done To My Gallbladder?
The gallbladder is sent to the pathologist. He/she carefully cuts and examines it under a microscope. This confirms the diagnosis, and excludes the presence of any growths, which occasionally co-exist. You will receive a full report from the pathologist after 1- 2 weeks, which you should show to your surgeon for final confirmation.
When Should I Call My Doctor After Surgery?
Call your doctor if:
- You develop a fever.
- You develop an unusual degree of pain
- You develop nausea or vomiting or cannot eat properly
- You become jaundiced (yellow eyes, dark urine)
Can People Manage Without A Gall Bladder?
Yes. If there is no gall bladder, bile just dribbles continuously into the intestine, rather than being reserved purely for after meals, as is the case if the gall bladder is functioning normally. There is no problem with digestion and people do not have any after-effects from their gall bladder having been removed.
Above information will help you to make an informed decision but it cannot replace the professional advice and expertise of a doctor who is familiar with your condition. You may have questions that are not covered; you should discuss these with your surgeon. You must remember every individual is different.
Doctors Dealing With Gall Stone Disease That You May Meet
Endoscopist: This may be a gastroenterologist or a surgeon who is able to undertake endoscopy (examination of the stomach or bowel using a flexible telescope). A few endoscopists can also perform ERCP and EUS, which are special forms of endoscopy that examine the biliary and pancreatic ducts and the pancreas
Gastroenterologist: A physician who is highly specialised in ‘gut’ problems.
General physician: A consultant medical doctor who works in a hospital and who is broadly specialised including ‘gut’ problems.
General surgeon: A consultant surgeon who works in a hospital and who is broadly specialised including ‘gut’ problems.
HepatoPancreatoBiliary surgeon: A surgeon who is highly specialized in pancreato-biliary & liver operations.
Glossary
MRI - Magnetic Resonance Imaging: A type of scanning performed to diagnose problems not picked up by regular investigations
CT SCAN – Computerized Tomography: A type of scanning performed to diagnose problems not picked up by regular investigations
ERCP – Endoscopic Retrograde Cholangiography: An endoscopic procedure performed to visualize bile & pancreatic ducts & treat the disease endoscopically whenever possible
EUS - Endoscopic UltraSound: An endoscopic procedure performed to visualize pancreas & biliary tract from very close, diagnose problems, obtain biopsies and at times treat the disease too.
MRCP – Magnetic Resonance Cholangio-Pancreatography: A special type of MRI performed to visualize bile & pancreatic ducts.
For Consultation Available At:
Timing: Monday To Friday - 9am To 5pm & Saturday 9am To 2pm
(Consultation Only by Appointment)
Address: Lilavati Hospital, A-791, Bandra Reclamation Rd, Bandra West, Mumbai, Maharashtra 400050
For Appointment call: 09821046391
Timing: Saturday 9am To 10am
(Consultation Only by Appointment)
Address: 93, ACI Hospital, 95, August Kranti Rd, Kemps Corner, Cumballa Hill, Mumbai, Maharashtra 400036
For Appointment call: 09821046391
Consultation Only by Appointment
Address: Raheja Rugnalaya Marg, Mahim West, Mahim, Mumbai, Maharashtra 400016

