Appointment Timing - 9am to 6pm
Portal vein resection during curative resection of pancreatic cancer
52-year old male patient presented with acute onset jaundice. He was a known case of with chronic calcific pancreatitis secondary to alcohol since 6 months with his gastroenterologist. He had steatorrhea and diabetes due to CP. He was on pancreatic enzyme supplements & insulin for the same. His investigations showed direct hyperbilirubinemia on blood investigations and dilated intrahepatic biliary radicles, CBD and PD on USG. Further investigations revealed significantly elevated levels of serum CA19-9 and a suspicious pancreatic mass on CT scan. It was probably involving the portal vein. However there was no evidence of distant metastasis.
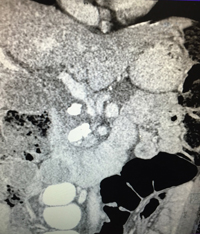
PIC-1
At this point patient came to LPC. A dedicated triple phase pancreas protocol CT scan of abdomen and pelvis showed a malignant appearing mass in uncinate process, causing circumferential narrowing of proximal superior mesenteric vein near its formation with jejunal vein (pic 1). Superior mesenteric artery however was free and there was no evidence of any further metastasis. This was a case of borderline resectable pancreatic cancer. A decision of surgery was taken after talking to the patient and family
Nature of surgery involved a complex pancreatoduodenal resection with resection of proximal superior mesenteric vein followed by its reconstruction. This was a very difficult reconstruction and carried a risk of requiring a simultaneous partial transverse colectomy. Also it carries a risk of major small bowel venous gangrene if reconstruction is not possible on table or it fails. On table the cancer was proven with frozen section analysis from a true-cut pancreatic biopsy. This was followed by a meticulous pancreatoduodenectomy using a superior mesenteric artery 1st approach. In this SMA is dissected 1st from the uncinate process upwards leaving the specimen attached to the PV/SMV. SMV was involved near uncinate process (pic 2).

PIC-2
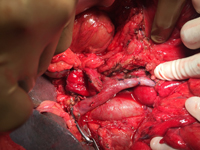
PIC-3
However it was free just above its union with 2nd jejunal vein and was looped here. The middle colic vein was sacrificed for mobilization and tumor free margin. However the transverse colon was still well vascularized. When specimen was removed the proximal portal vein with draining splenic vein stump was available for anastomosis with stump of 2nd jejunal vein and SMV. A venoplasty was done between the 2nd jejunal vein and SMV to create one lumen. This was anastomosed with the PV. (Pic 3) The remaining reconstruction between pancreas, bile duct and jejunum was done in the standard fashion. Postoperative Doppler study showed good flow in the PV. Patient recovered well after surgery and was discharged on POD 15.
HP showed involvement of the SMV wall sparing the intima. 4 weeks later patient was started on adjuvant chemotherapy. He is doing well 6 months post surgery without any recurrence. This is an example of how a complex vascular resection reconstruction can salvage borderline resectable cases of pancreatic cancer.
Points to remember:
- Borderline resectable pancreatic cancer (BRPC) is a one of the most difficult disease to treat for a pancreatic cancer surgeon
- Borderline resectable pancreatic cancer includes patients with involvement of portal or superior mesenteric vein by the tumor, <180 degree abutment of SMA, involvement of GDA up to its origin from HA or mesocolon involvement
- Surgery involves pancreatoduodenectomy with regional lymph node dissection, with vascular resection & reconstruction with or without additional bowel resection.
- Vascular resection is done for portal or proximal SMV involvement.
- Venous reconstruction may involve a vascular interposition graft placement.
- Arterial reconstruction of SMA is not advocated. However a reconstruction of segment of HA may be done occasionally.
- Surgery is followed by chemotherapy / chemo radiotherapy
- Surgery in high volume pancreatic surgery with experience in complex multivisceral resection, vascular resection and reconstruction offers the best results.
- Radical surgery followed by chemo radiation gives good chances of long-term survival.
Disclaimer: The views expressed in this article solely belong to the author. The information provided here is for Educational and informational purposes only.
This newsletter is for private circulation only.
