Appointment Timing - 9am to 6pm
Liver Cyst
This is a patient information booklet providing specific practical information about liver cysts in brief. Its aim is to provide the patient & his or her family with useful information on this particular liver problem, the procedures and tests you may need to undergo, treatment approaches, risks involved, duration, expenses and helpful advice on coping successfully with the problem. If you require more information, Dr. D.R.Kulkarni or your doctor will be able to provide more information.
Click Here For Quick Links of Article
- What Is Liver?
- Liver Function
- What Are The Tests To Check Liver Function?
- What Is A Cyst?
- Why Do Cysts Form In Liver?
- Can Liver Cysts Be Inherited?
- How Common Are Liver Cysts?
- How Do They Present?
- How Is A Patient With Liver Cyst Evaluated?
- How Is A Patient With Liver Cyst Evaluated?
- When Should Liver Cyst Be Treated?
- How Are They Treated?
- What Are The Surgical Options?
- Can The Surgery Be Done Laparoscopically?
- Which Anesthesia Will Be Used?
- How Many Ports Are Used?
- Will The Cyst Be Removed Completely Or Partially?
- What Will Be The Postoperative Course?
- What Is The Follow Up Schedule?
- What Postop Complications Are Possible?
- What Is Done For PCLD?
- What Is The Long Term Outcome?
- What Is Done For Cystic Tumors Of Liver?
- Hydatid Cysts
- What Causes Hydatid Cyst?
- How Does The Cyst Form?
- Are Symptoms Diferrent?
- What Are The Complications Of Hydatid Cyst?
- What Is The Treatment Of Hydatid Cysts?
- Indications for PAIR
- Contraindications for PAIR
- Doctors Dealing With Liver Disease That You May Meet
What Is Liver?
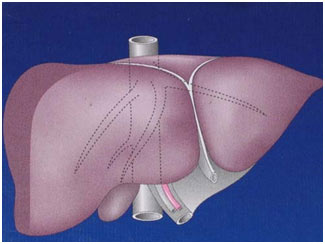
The human liver is a reddish brown organ normally weighing approximately 1.5% of body weight. It is the largest internal organ. It is located in the right upper part of the abdominal cavity, resting just below the diaphragm under the protection of rib cage. Liver is broadly divided into a large right and a relatively small left lobe. Additionally there is a small lobe called caudate lobe. The right and left lobes are further subdivided into segments. These subdivisions help in planning liver surgery when a patient needs removal of a portion of liver.
Apart from a patch where it connects to the diaphragm the liver is covered entirely by peritoneum, a thin, double-layered membrane that reduces friction against other organs. The peritoneum folds back on itself to form the falciform ligament and the right and left triangular ligaments. These "ligaments" are in no way related to the true anatomic ligaments in joints, and have essentially no functional importance. An exception to this is the falciform ligament, which attaches the liver to the anterior body wall from within.

Liver is supplied by two large blood vessels, one called the hepatic artery and one called the portal vein. The hepatic artery carries blood from the aorta, whereas the portal vein carries blood containing digested nutrients from the entire gastrointestinal tract and also from the spleen and pancreas. The hepatic portal vein supplies approximately 75% of the liver's blood supply, the hepatic artery accounting for the remainder of its blood flow. Oxygen is provided from both sources.
Before entering the liver the portal vein and hepatic artery divide into right and left branch for each of the lobes. They further subdivide within the liver tissue to supply each segment in total 9 in number. Blood flows through channels called sinusoids and empties into the central vein of each lobule. (Each lobule is made up of millions of hepatic cells, which are the basic metabolic cells.). The central veins coalesce into hepatic veins, which leave the liver. There are 3 main hepatic veins that drain blood from liver into a large vein (inferior vena cava), which carries blood from lower portion of body to heart. Apart from the 3 main Hepatic Veins there are many smaller draining veins, which enlarge if any or all of the 3 veins are blocked due to diseases like cirrhosis or hepatic vein thrombosis or veno- occlusive disorders.
The caudate lobe is a separate structure, which receives blood flow from both the right- and left- sided vascular branches and then drains through small veins directly into the vena cava.
The bile produced in the liver is collected in bile canaliculi, which merge to form bile ducts. Bile ducts are tube like structures carrying bile produced within liver to the intestine. Within the liver, these ducts are called intrahepatic (within the liver) bile ducts, and once they exit the liver they are considered extrahepatic (outside the liver). The intrahepatic ducts eventually drain into the right and left hepatic ducts, which merge to form the common hepatic duct. The term biliary tree is derived from the arboreal branches of the bile ducts. The cystic duct draining the gallbladder joins with the common hepatic duct to form the common bile duct. Bile can either drain directly into the duodenum via the common bile duct, or be temporarily stored in the gallbladder via the cystic duct. The common bile duct and the pancreatic duct enter the second part of the duodenum together at the ampulla of Vater.
The liver has a "capsule" around it, which contains nerve endings, accounting for pain when the liver enlarges and stretches its capsule. The damaged liver has an amazing ability to regenerate itself. The body needs only about 20% of the liver to live, and if a piece is cut out or injured, it can grow back. Sometimes, however, the liver gets chronic diseases, which impair its ability to regenerate. It can become infiltrated with fat ("steatosis"), shrink from chronic alcohol or viral exposure ("cirrhosis") or grow large from infection or a blocked blood drainage ("hepatomegly"). Any inflammation of the liver, whether caused by germs, drugs, or radiation, is called hepatitis. A damaged liver may heal, or may slowly fail and require liver transplant to save the patient's life.
What Is The Function Of Liver?
The liver is an astounding laboratory sustaining metabolism. Liver's main job is to filter the blood coming from the digestive tract, before passing it to the rest of the body. The liver detoxifies chemicals and metabolizes drugs. As it does so, the liver also secretes bile that ends up back in the intestines. Bile contains bile salts, which are responsible for digestion and absorption of food material. The liver is responsible for carbohydrate, fats & protein metabolism and also makes albumin, proteins important for blood clotting and other functions. It also produces various clotting factors, stores glucose, fats, vitamins like A, D3, B12 & minerals like iron & copper. This myriad of functions makes clear why the liver is essential to life.
What Are The Tests To Check Liver Function?
The diagnosis of liver function is made by blood tests. Liver function tests can readily pinpoint the extent of liver damage. Usually in liver diseases patient can have a combination of raised bilirubin, increase in liver enzymes, drop in blood albumin levels, alteration in clotting test results, depending on the type of liver disease.
If liver function is altered then other tests are asked depending on clinical picture and lab results. If hepatitis is suspected, then tests to detect cause of hepatitis are done. Sometimes, one may require an ultrasound or a CT scan or MRI to produce images of the liver and diagnose liver tumors, abscess, and other pathologies.
Physical examination of the liver is not accurate in determining the extent of liver damage. It can only reveal presence of tenderness or the size of liver, but in most cases, some type of radiological study is required to examine it. In patients with chronic liver disease noninvasive tests like Phytate liver scan (nuclear scan) and Ultrasound elastography of liver (Fibroscan) are done to assess the liver status.
However, the ideal way to determine damage to the liver is with a biopsy. A biopsy is not required in all cases, but may be necessary when the cause or extent of damage is unknown. A needle is inserted into the skin just below the rib cage and a biopsy is obtained. The tissue is sent to the laboratory, where it is analyzed under a microscope. Sometimes, a radiologist may assist the physician performing a liver biopsy by providing ultrasound guidance.
What Is A Cyst?
A cyst is a collection of fluid bound by defined wall either of surrounding tissue or a lining. When the cyst has a lining from within also called epithelium, it is known as true cyst in medical terms and if there is no lining it is known as false or pseudo cyst.
Cyst can be present anywhere in the body whether in brain, lung, liver, kidney, pancreas, spleen, abdominal cavity, ovary, and neck etcetera. Pseudo cysts however are specifically seen originating from pancreas or as a result of pancreatic inflammation.
Why Do Cysts Form In Liver?
A cyst can form in the liver due to various causes. They can be due to congenitally obstructed small biliary channels within liver and have lost communication with others. These are Simple Liver Cysts (SLC) and are by far the commonest of liver cysts. They are never inherited. SLC might be single or many scattered cysts.
Sometimes a cyst forms due to parasitic infections (ecchinococcus or tapeworms) and is known as hydatid cysts. Occasionally a cyst is actually a benign tumor called biliary cyst- adenoma or a cancer called cystadeno- carcinoma the cause of cystadenomas and cystadeno- carcinomas is unknown. It is important to know that Cystadenoma is a premalignant lesion & can transform to cyst- adenocarcinoma. Sometimes a liver cancer with central destruction can also give appearance of a cyst.
Rarely multiple cysts are result of congenital malformation of bile ducts (choledocal cyst & caroli disease) or residual collection following an abscess or trauma.
Can Liver Cysts Be Inherited?
Less commonly liver cyst can be part of hereditary diseases like polycystic disease wherein multiple cysts occur in organs like kidney, liver, pancreas. Adult polycystic liver disease (AD-PCLD) is congenital & inherited disorder and is usually associated with autosomal dominant polycystic kidney disease (AD-PKD). Mutations in these patients have been identified in PKD1 and PKD2 genes. Occasionally, PCLD has been reported in the absence of polycystic kidney disease (PKD). In these patients, a third gene, protein kinase C substrate 80K-H (PRKCSH), has been identified.
Despite these differences in genes, patients with PCLD are similar in clinical presentation. In patients with PKD, the kidney cysts usually precede the liver cysts. PKD often results in renal failure, whereas liver cysts only rarely are associated with hepatic fibrosis and liver failure.
In an autosomal dominant inherited disease there is 50% chance of disease occurring in the child if one parent is having the disease. If both parents have it the risk increases to 75%. In case of autosomal recessive disorder there is only 25% risk of child getting the disease only if both the parents are having the diseased chromosome.
How Common Are Liver Cysts?
Liver cysts tend to occur in 5% of the population. No more than 10-15% of these patients have symptoms. Hepatic cysts are usually found as an incidental finding on imaging or at the time of laparotomy.
How Do They Present?
Liver Cyst especially simple liver cyst generally causes no symptoms and is usually picked up when an abdominal ultrasonography is performed for abdominal complaints. Imaging studies often reveal asymptomatic lesions incidentally. What is important to remember is that a malignant liver cyst would most of the times present in the same way as a simple liver cyst.
A liver cyst of any etiology causes complaints only when it is large in size, causes pressure on surrounding organs or develops complications like bleeding, infection rupture or cancer.
Cyst may produce dull right sided abdominal pain, bloating and early satiety if large in size. Occasionally, a cyst is large enough to produce a palpable abdominal mass. Jaundice caused by bile duct obstruction is rare. Patient may develop secondary infection, leading to a presentation similar to a hepatic abscess with abdominal pain & fever. Free rupture in the abdomen or within the biliary system or bleeding inside the cyst causes acute severe abdominal pain.
Can Liver Cysts Cause Liver Failure?
Most liver cysts will not cause liver failure. Rarely patients with PCLD present with symptoms of portal hypertension & liver failure like hematemesis (blood vomiting), ascites (accumulation of water in the abdomen), encephalopathy (loss of consciousness).
How Is A Patient With Liver Cyst Evaluated?
Cysts can usually be distinguished on the basis of the patient's symptoms, the radiographic appearance of the lesion, certain blood tests and analysis of the cyst fluid. It is important to identify the exact nature of the cyst.
A simple cyst, a hydatid cyst & cystic tumor in its early stage of disease would appear same. A practical problem in the evaluation of a patient with a cystic hepatic lesion is differentiating cystic neoplasms from simple cysts.
Also it is important to find out whether your complaints are due to some other cause, which will be the situation most of the times in case of simple liver cyst. It is a different situation when a patient presents with a complication of liver cyst like hemorrhage or infection or when cyst is very large (>7cms)
Therefore evaluation of a patient with a liver cyst involves carefully recording patient history and performing a physical examination. If necessary laboratory investigations including a complete blood count, renal function tests like blood urea nitrogen & creatinine, liver function tests, immunological tests (blood tests) to rule out hydatid disease, tumor markers like CA19-9 are done. Sometimes cyst fluid is aspirated under utrasonography guidance for analysis to rule out a cancer. An imaging study, such as an abdominal CT scan or MRI is done if the cyst is large, to define the nature & anatomy of the cyst.
In case of small simple liver cyst the diagnosis is completed after a routine abdominal ultrasonography and no follow up study or consultations is necessary. Liver function test results, such as transaminases or alkaline phosphatase or bilirubin are usually normal in case of simple cysts. Liver function test abnormalities like raised liver enzymes and bilirubin would occur only if cyst is large and causes pressure on the bile ducts. Coagulation profile is usually within the reference range. Percutaneous aspiration is avoided because the laboratory and cytologic evaluation of the simple cyst fluid is nondiagnostic, and a small risk exists of inducing anaphylaxis from leakage if cyst is a hydatid cyst or of causing abscess formation in a previously sterile cyst.
Abnormalities in LFT can occur more frequently in case of PCLD or Hydatid cyst because of pressure on the bile ducts or rupture of hydatid material in the bile duct. In the presence of hydatid cysts, high eosinophil count is noted in approximately 40% of patients in routine CBC, and echinococcal antibody titers are positive in nearly 80% of patients.
As with simple cysts, liver function test results are normal with cystic tumors. There may be mild abnormalities in some patients. Carbohydrate antigen (CA) 19-9 levels are elevated in some patients. Cyst fluid can be sent for CA 19-9 testing as a marker for cystadenoma and cystadenocarcinoma
In the setting of PCLD, greater abnormalities in liver function test results are found, but liver failure is uncommon and is usually seen in very advanced disease with liver fully riddled with large cysts compressing the bile ducts and blood vessels. Renal function test results, including blood urea nitrogen and creatinine levels, are often abnormal and should be performed on initial evaluation.
When Should Liver Cyst Be Treated?
- Small simple hepatic cysts do not require any therapy.
- Even large but asymptomatic simple liver cysts do not require therapy.
- Only symptomatic simple liver cysts usually larger than 7 cms in size may require treatment.
- Hydatid cyst, suspected or confirmed cystadenoma or cystadenocarcinoma should always be treated
How Are They Treated?
Simple liver cyst can be treated with aspiration (PAIR) method or surgery. There is no medical treatment for simple liver cyst.
Percutaneous aspiration under ultrasound or CT guidance is avoided because the recurrence rates are nearly 100%. Typically, the fluid within a simple liver cyst is light yellow in color. The cyst fluid is continually secreted by the epithelial lining of the cyst. For this reason, needle aspiration of simple cysts is not curative.
Sometimes however a large cyst is aspirated just to find out if it relieves complaints, in which case a definitive treatment can be taken up later if the cyst refills.
Aspiration combined with instillation of alcohol or other chemical agents is done in some patients. This method is known as PAIR (Percutaneous Aspiration Instillation & Reaspiration). These chemical agents are called sclerosants and they destroy the inner lining of the cyst thereby preventing further secretion of fluid and recurrence.
But this method has high failure and recurrence rates. Successful sclerosis depends on complete decompression of the cyst, complete destruction of cyst lining and apposition of the cyst walls. This is not possible if the cyst wall is thickened or if the cyst is large. Additionally there is risk of the sclerosing agent slipping down into the bile ducts causing permanent damage called sclerosing cholangitis.
Percutaneous catheters should not be placed to drain simple cysts because the cavity becomes contaminated, leading to the development of hepatic abscess. Unlike the typical pyogenic hepatic abscess, this problem is difficult to resolve with repeated catheter placements because of continued secretion from the cyst epithelium. This would eventually require surgery.
What Are The Surgical Options?
Surgical treatment of simple liver cysts involves "unroofing" the cyst by excising a portion of the wall that extends above the surface of the liver. Excision of this portion of the cyst wall at the liver surface produces a saucer-type appearance in the remaining cyst so that any fluid secreted from the remaining epithelium leaks into the peritoneal cavity where it can be absorbed from a much larger surface. Although ablating the remaining epithelium with electrocautery or an argon beam coagulator is possible, this generally is not required because the volume of fluid secreted each day can be absorbed by the peritoneum without any consequence. Additionally it has the risk of damaging underlying bile ducts.
Can The Surgery Be Done Laparoscopically?
Yes, cyst deroofing can be successfully performed laparoscopically. The laparoscopic approach is currently considered the standard of care. When compared to laparotomy, this technique is associated with less postoperative pain and disability,
Histologic assessment of the excised cyst wall should be routinely undertaken to identify the presence of an unsuspected neoplasm, such as cystadenoma.
If cysts on imaging studies show abnormalities suggestive of cystic tumors, or are of equivocal etiology surgery is indicated. Other surgical indications include large cysts at risk of rupture and abscesses not anatomically amenable to percutaneous treatment.
Which Anesthesia Will Be Used?
General anesthesia is the norm. Prophylactic antibiotics are not necessary. Sometimes an orogastric tube and urinary catheter is necessary
How Many Ports Are Used?
3 or 4 ports are used for laparoscopic cyst surgery.
Will The Cyst Be Removed Completely Or Partially?
Excision of the entire cyst wall is neither necessary nor desired and, if attempted, carries the risk of injury to portal or hepatic venous vessels that may be stretched over the cyst wall.
What Will Be The Postoperative Course?
A light diet is offered the evening of surgery, and most patients can be discharged home the following day.
Generally, recovery is rapid, and most patients resume full activity within 1 week. Patients can shower with the waterproof dressings in place the day after surgery. The dressings can be removed after 2-3 days.
What Is The Follow Up Schedule?
Following successful laparoscopic unroofing of a simple liver cyst, the patient is seen at a follow- up visit within 2 weeks and again 6 weeks after surgery to assess symptomatic relief and to identify complications, such as wound infection or ascites.
Routine radiographic studies are not obtained unless symptoms recur.
What Postop Complications Are Possible?
Complications of laparoscopic unroofing of simple liver cysts are uncommon. Trocar site infection is a rare occurrence. Unexpected leakage of bile from the cut edges of the cyst can lead to a subhepatic or subphrenic fluid collection or, rarely, bile ascites.
In patients with PCLD, unroofing and fenestration procedures can cause injury to biliary or vascular structures in the compressed hepatic parenchyma between the cysts.
In patients with hydatid cysts, spillage of cyst contents into the peritoneal cavity may cause anaphylaxis. This can even give rise to disseminated hydatid disease in peritoneum.
What Is Done For PCLD?
Treatment of PCLD is indicated only in symptomatic patients. Asymptomatic patients do not require therapy because the risk of developing complications related to the lesion is lower than the risk associated with treatment.
No options are available for the medical treatment of PCLD. In AD-PCLD, enlargement of the liver occurs slowly and only rarely compromises liver function. Only patient with clearly disabling pain is considered for surgery and as much of the cystic liver as possible is decompressed. This is accomplished by a combination of unroofing and fenestration (drilling holes) or, in selected patients, by resection of the involved portion of the liver. Recurrence of symptoms with either procedure is high as new cysts replace those that have been resected. Small numbers of patients need liver transplantation.
What Is The Long Term Outcome?
Laparoscopic unroofing of simple hepatic cysts have reported cure rates of 90% or higher. In patients with simple liver cysts, the general agreement is that laparoscopic unroofing offers the best balance between efficacy and safety.
Patients with PCLD have lower cure rates. How patients with PCLD should be treated remains less clear because the failure rates for laparoscopic unroofing and fenestration are high. Liver resection, though more effective, carries higher risks.
What Is Done For Cystic Tumors Of Liver?
Cystadenoma and cystadenocarcinoma always need surgery as the treatment. Quite often these pathologies are diagnosed on histopathology after the first surgery like deroofing. A second curative surgery is then required. Several surgical methods for treatment of cystadenoma and cystadenocarcinoma have been described. Regardless of surgical technique, all surgical options should result in complete ablation of the tumor. Enucleation and formal resection have been accepted as appropriate treatment options. Fenestration and complete fulguration have also been implemented, although, in this method, complete ablation cannot be confirmed by pathology.
Hydatid Cysts
What Causes Hydatid Cyst?
Hydatid cysts are caused by parasite Echinococcus granulosus. Which is a tapeworm. This parasite is found worldwide, but it is particularly common in areas of sheep and cattle farming.
How Does The Cyst Form?
The adult tapeworm lives in the digestive tract of carnivores, such as dogs or wolves. Eggs are released into the stool and are inadvertently ingested by the intermediate hosts, such as sheep, cattle, or humans. The egg larvae invade the bowel wall and mesenteric vessels of the intermediate host, allowing circulation to the liver. In the liver, the larvae grow and become encysted. This is the hydatid cyst. The hydatid cyst develops an outer layer of inflammatory tissue and an inner germinal membrane that produces daughter cysts. When carnivores ingest the liver of the intermediate host, the scolices of the daughter cysts are released in the small intestines and grow into adult worms, thus completing the life cycle of the worm.
Are Symptoms Diferrent?
Patients with hydatid cysts, similar to patients with simple cysts, are most often asymptomatic, but pain may develop as the cyst grows. Larger lesions typically cause pain and are more likely to develop complications than simple cysts. At the time of presentation, patients generally have a palpable mass in the right upper quadrant.
What Are The Complications Of Hydatid Cyst?
Cyst rupture is the most serious complication of hydatid cyst. Cysts may rupture into the biliary tree, through the diaphragm into the chest, or freely into the peritoneal cavity. Rupture into the biliary tree may result in jaundice or cholangitis. Free rupture into the peritoneal cavity may cause anaphylactic shock. Also many more cysts would form in the peritoneal cavity. As with simple cysts, patients with hydatid cysts may develop secondary infection and subsequent hepatic abscesses.
What Is The Treatment of hydatid cysts?
Patients with hydatid cysts should be treated to prevent complications related to cyst growth and rupture.
Medical therapy with antihydatid agent albendazole is treatment of choice in small cysts. Usually these patients will not need any other therapy. Patients with larger and complicated cysts require surgery. In surgically treated patients, albendazole is generally given for few weeks pre and postoperatively; continuation is limited to those who have spillage of cyst fluid at the time of operation or to those with cyst rupture.
Antihydatid agents are used in conjunction with percutaneous treatment. Medical therapy should be started 4 days prior to percutaneous treatment and continued either for 1 month (albendazole).
PAIR (puncture, aspiration, injection, reaspiration) is a percutaneous treatment technique for hydatid disease. In this minimally invasive method, a needle is introduced into the cyst under ultrasound guidance. Cyst fluid is aspirated and analyzed. Hypertonic saline or ethanol is then injected and reaspirated. PAIRD (puncture, aspiration, injection, reaspiration, drainage) is similar to PAIR except that a catheter is left in place after completion of the procedure. PAIRD is most often used for large cysts.
Patients should be followed clinically after PAIR treatment. Recurrence is increased in more complicated cysts, including those with multiple daughter cysts.
PAIR is performed only in highly specialized centers with appropriately trained and experienced staff. In addition, an anesthesiologist should be present for monitoring and treatment in the event of anaphylactic shock. Surgeons should be notified immediately in case of complication.
The World Health Organization currently supports PAIR as an effective alternative to surgery, although its use is limited.
The World Health Organization guidelines for indications and contraindications of PAIR are as follows:
Indications for PAIR
- Nonechoic lesion greater than or equal to 5 cm in diameter
- Cysts with daughter cysts and/or with membrane detachment
- Multiple cysts if accessible to puncture
- Infected cysts
- Patients who refuse surgery
- Patients who relapse after surgery
- Patients in whom surgery is contraindicated
- Patients who fail to respond to drug therapy alone
- Children older than 3 years
- Pregnant women
Contraindications for PAIR
- Noncooperative patients
- Inaccessible or risky location of the liver cyst
- Cyst in spine, brain, and/or heart
- Inactive or calcified lesion
- Cyst communicating with the biliary tree (In patients who are jaundiced with hydatid disease, endoscopic retrograde cholangiopancreatography (ERCP) or MRCP is done to see if the cyst has ruptured/communicating into the bile duct.)
More complicated cysts are better managed surgically. Treatment of hydatid cysts is associated with 2 technical problems: risk of anaphylaxis from spillage of cyst fluid containing eggs and larvae into the peritoneal cavity and recurrence caused by residual eggs in incompletely removed germinal membranes.
To prevent these problems, most surgeons use a technique in which the cyst contents are aspirated and replaced with a hypertonic saline solution to kill residual daughter cysts in the germinal membrane before unroofing and pericystectomy. The goal of the latter procedure is to excise the germinal membrane, leaving the inflammatory and fibrous components of the cyst wall in situ. Excision of the entire cyst wall or formal hepatectomy is used selectively.
Note: Above information will help you to make an informed decision but it cannot replace the professional advice and expertise of a doctor who is familiar with your condition. You may have questions that are not covered; you should discuss these with your surgeon. You must remember every individual is different.
Doctors Dealing With Liver Disease That You May Meet
Endoscopist: This may be a gastroenterologist or a surgeon who is able to undertake endoscopy (examination of the stomach or bowel using a flexible telescope). A few endoscopists can also perform ERCP and EUS, which are special forms of endoscopy that examine the biliary and pancreatic ducts and the pancreas
Gastroenterologist: A physician who is highly specialized in ‘gut’ problems.
General physician: A consultant medical doctor who works in a hospital and who is broadly specialized including ‘gut’ problems.
General surgeon: A consultant surgeon who works in a hospital and who is broadly specialized including ‘gut’ problems.
HepatoPancreatoBiliary surgeon: A surgeon who is highly specialized in pancreato-biliary & liver operations.
Glossary
MRI - Magnetic Resonance Imaging A type of scanning performed to diagnose problems not picked up by regular investigations
CT SCAN - Computerized Tomography A type of scanning performed to diagnose problems not picked up by regular investigations
ERCP – Endoscopic Retrograde Cholangiography. An endoscopic procedure performed to visualize bile & pancreatic ducts & treat the disease endoscopically whenever possible
EUS -Endoscopic UltraSound. An endoscopic procedure performed to visualize pancreas & biliary tract from very close, diagnose problems, obtain biopsies and at times treat the disease too.
MRCP – Magnetic Resonance Cholangio- Pancreatography
For Consultation Available At:
Timing: Monday To Friday - 9am To 5pm & Saturday 9am To 2pm
(Consultation Only by Appointment)
Address: Lilavati Hospital, A-791, Bandra Reclamation Rd, Bandra West, Mumbai, Maharashtra 400050
For Appointment call: 09821046391
Timing: Saturday 9am To 10am
(Consultation Only by Appointment)
Address: 93, ACI Hospital, 95, August Kranti Rd, Kemps Corner, Cumballa Hill, Mumbai, Maharashtra 400036
For Appointment call: 09821046391
Consultation Only by Appointment
Address: Raheja Rugnalaya Marg, Mahim West, Mahim, Mumbai, Maharashtra 400016

