Appointment Timing - 9am to 6pm
Liver Hemangioma / Hepatic Hemangioma
This is a patient information booklet providing specific practical information about hepatic hemangioma in brief. Its aim is to provide the patient & his or her family with useful information on this particular liver problem, the procedures and tests you may need to undergo, treatment approaches, risks involved, duration, expenses and helpful advice on coping successfully with the problem. If you require more information, Dr. D.R.Kulkarni or your doctor will be able to provide more information.
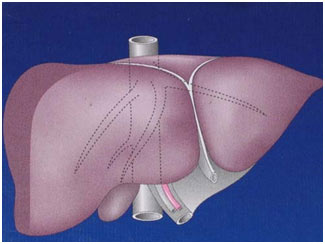
Hemangioma
A hemangioma is a noncancerous tumor made of widened (dilated) blood vessels that are atypical or irregular in arrangement and size. These vascular spaces may contain thrombin, calcifications, or prominent scarring (sclerosed hemangioma). Phleboliths are rare. Grossly, these lesions often appear as having a flat surface or as bulging subcapsular lesions. Lesions are reddishblue and well demarcated from surrounding tissue. Large tumors may become pedunculated.
How Common Is Liver Hemangioma?
Hemangioma is the most common benign tumor affecting the liver. The widespread use of noninvasive abdominal imaging modalities has led to increased detection of it even when it is asymptomatic.
What Is A Giant Hemangioma?
Giant hemangiomas are large hemangiomas and the size definition actually varies in the books but commonly anything more than 5cms is considered giant hemngioma.
What Causes A Hemangioma In Liver?
It’s not clear what causes a liver hemangioma to form. It is probably congenital — meaning that you’re born with it. It is certainly not familial or genetically inherited. Some associations are observed regarding occurrence and growth of a hemangioma like age, sex, hormonal influence, drugs etcetera.
Women, especially with a history of multiparity, are affected more often than men. Women who have been pregnant are more likely to be diagnosed with a liver hemangioma than women who have never been pregnant. Women who used hormone replacement therapy for menopausal symptoms may be more likely to be diagnosed with liver hemangioma than women who did not.
Several pharmacologic agents have been postulated to promote its growth. Steroid therapy , estrogen therapy, and pregnancy can increase the size of an already existing hemangioma.
Hepatic hemangiomas can occur at all ages. Most hepatic hemangiomas are diagnosed in individuals aged 30-50 years. Female patients often present at a younger age and with larger tumors. Hepatic hemangiomas may be seen in
infancy. They have also been detected prenatally in a growing fetus. Babies may develop a type of hepatic hemangioma called benign infantile hemangioendothelioma. This rare, noncancerous tumor has been linked to high rates of heart failure and death in infants. Infants are usually diagnosed by the time they are 6 months old. Hepatic hemangiomas may be seen in 5-10% of children aged 1 year. They typically regress during childhood.
What Are The Symptoms And Signs?
Hemangiomas of the liver are usually small and hence asymptomatic. However, even large hemangiomas remain asymptomatic most often. Most cases of liver hemangioma are discovered during a test or procedure for some other
condition. Most people who have a liver hemangioma never experience symptoms, never show signs and most hemangiomas don’t grow even over long periods or have complications and hence may never need treatment.
But in a small number of people, liver hemangioma will grow, may cause symptoms or complications and require treatment. It’s not clear why this happens. Larger, especially more than 10cms and multiple lesions may produce
symptoms.
Dull pain, vague discomfort, which cannot be explained in words or fullness in the right upper abdomen, is the most common complaint especially when it is located in the right lobe of liver. Hepatic hemangiomas are more common in
the right lobe of the liver than in the left lobe.
Early satiety (feeling full after eating even small amount of food), nausea, and vomiting may occur when large lesions compress the stomach, producing obstruction. This is more common with lesions located in the left side or those
hanging form liver like bunch of grapes.
Rarely, hemangiomas may present as a large abdominal mass. Other atypical presentations include jaundice from compression of the bile ducts, gastrointestinal bleeding, fever of unknown origin or cardiac failure.
In some cases, acute abdominal pain occurs due to various complications like clot formation inside the hemangioma (called thrombosis), hemorrhage into the lesion or free intraabdominal cavity, twisting or torsion if there is a stalk for hanging hemangioma or compression of adjacent tissues or organs.
Consumption of coagulation factors causes an illness that resembles a systematic inflammatory process with findings of fever, weight loss, anemia, thrombocytosis, increased fibrinogen level, and elevated erythrocyte sedimentation
rate.
Babies with benign infantile hemangioendothelioma may have a growth in the abdomen, failure to survive or grow, anemia, and heart failure The only findings upon physical examination are, infrequently, an enlarged liver, a palpable abdominal mass or the presence of an arterial bruit over the right upper quadrant.
Do All Liver Hemangiomas Require Treatment?
Most hepatic hemangiomas are small and asymptomatic at the time of diagnosis, and they are likely to remain that way. In addition, malignant transformation has not been reported in hepatic hemangiomas. Even large hemangiomas have very little risk of complications. For these reasons, most asymptomatic hepatic hemangiomas are left safely alone.
For Consultation Available At:
Timing: Monday To Friday - 9am To 5pm & Saturday 9am To 2pm
(Consultation Only by Appointment)
Address: Lilavati Hospital, A-791, Bandra Reclamation Rd, Bandra West, Mumbai, Maharashtra 400050
For Appointment call: 09821046391
Timing: Saturday 9am To 10am
(Consultation Only by Appointment)
Address: 93, ACI Hospital, 95, August Kranti Rd, Kemps Corner, Cumballa Hill, Mumbai, Maharashtra 400036
For Appointment call: 09821046391
Consultation Only by Appointment
Address: Raheja Rugnalaya Marg, Mahim West, Mahim, Mumbai, Maharashtra 400016

