Appointment Timing - 9am to 6pm

Pancreatic Duct Stenting In Chronic Pancreatitis – Useful Or Harmful
Case:1
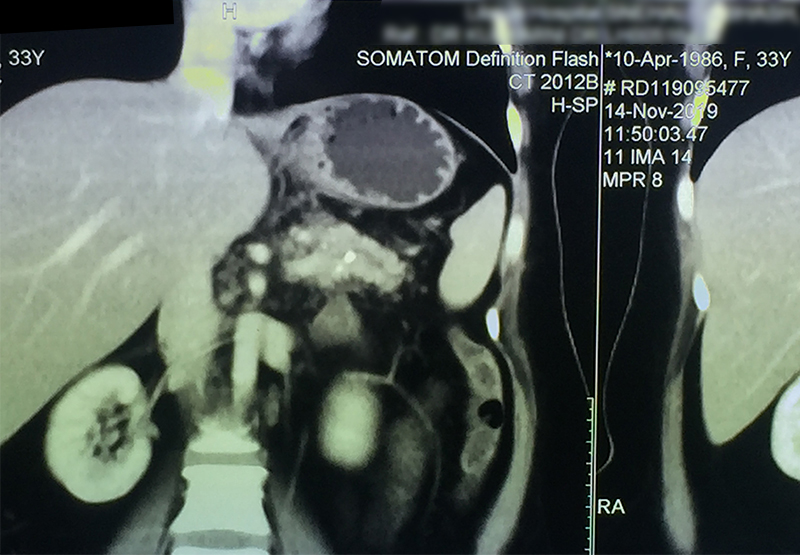
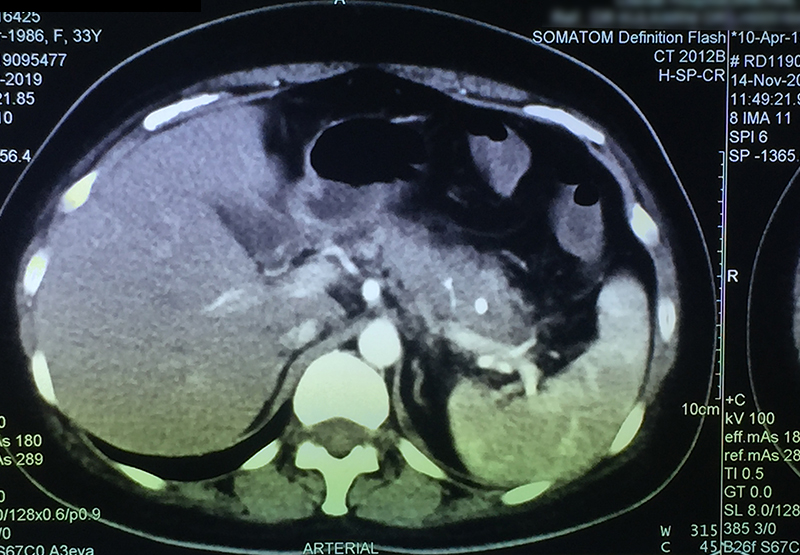
30 year old young lady with chronic pancreatitis, narrowing (stricture) of the pancreatic duct in the head and tail of pancreas and obstructing stone in the tail portion of the pancreatic duct presented to us with a recent attack of mild acute pancreatitis. She had undergone pancreatic duct stenting 3 times before this and stent migrated out of the duct at the last time following which she had acute pancreatitis. She was thoroughly evaluated with CT scan and MRI of abdomen. It showed that the duct had dilated irregularly in head and body of the pancreas and a stone was lodged in the tail. So she had disease both in the head and tail. She underwent a distal pancreatosplenectomy for the tail disease and a pancreaticojejunostomy (Head coring—Frey procedure) for the disease of the head and body of pancreas. She recovered well however the recovery was prolonged due to intra-abdominal infection caused by organisms in the infected pancreatic fluid. Infections originated from the pancreatic stents, were resistant to routine antibiotics and needed expensive drugs for infection control.
Case:2
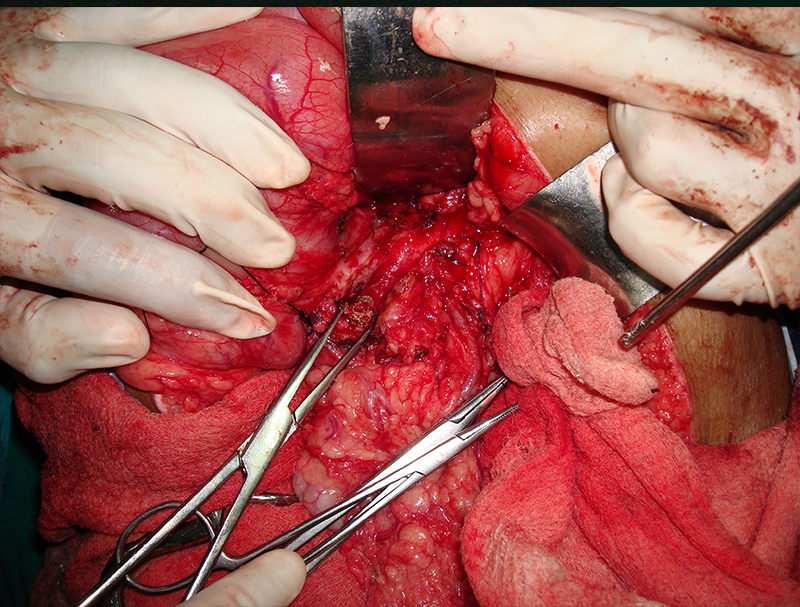
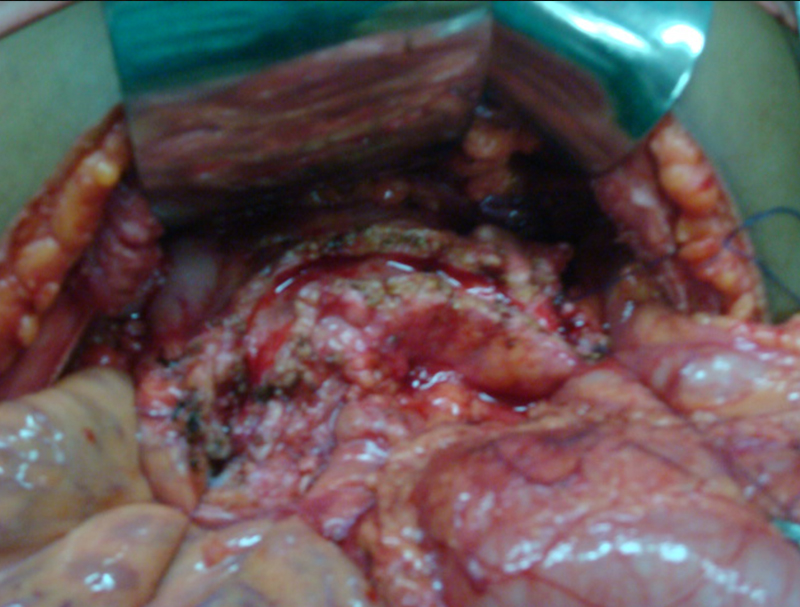
25 year old male presented with abdominal pain due to chronic calcific pancreatitis. He had had multiple previous endoscopic stent placement procedures & external shock wave treatment (ESWL) attempts to break & remove pancreatic stones and pancreatic duct stenting. He was investigated and later operated. A Frey procedure was done wherein the inflamed and stone filled core in the head of pancreas was removed, duct was widely opened along the head, neck, body and tail of pancreas. All the ductal stones were removed and multiple narrowing were opened. A loop of intestine was then joined with the pancreatic duct. He recovered uneventfully. He is fine for last 8 years and has not required any long term painkillers or had any episodes of pancreatitis. His dose of pancreatic enzyme supplements has also come down.
Case:3
40 year old male with chronic calcific pancreatitis due to alcohol, continuous abdominal pain and weight loss underwent surgery (head coring and pancreaticojejunostomy). He did not have any previous stenting procedures. Patient recovered smoothly and was discharged on 6th day after surgery and has remained well for last 6 years.
The above 3 cases are only few of the many such patients with chronic calcific pancreatitis treated at LPC some of who were previously stented for chronic pancreatitis ELSEWHERE and may have also received lithotripsy for pancreatic calculi. We would like to make it clear at the outset that pancreatic stenting is not a wrong treatment. However it also has to be made clear that pancreatic stents should be used very carefully. Else it only leads to multiple endoscopic sessions, significant expense, introduction of infective organisms in the pancreatic juice and finally a much needed surgical procedure filled with infective complications.
Why do patients undergo stenting?
The fear of major surgery, possible complications & expenses for the surgery versus hope of avoiding major surgery is the biggest reason for this. Also many patients are not aware that multiple sessions will be required with stents, stent may fail to give desired permanent outcome , stent can cause complications too and most importantly what are the correct indications.
What are the correct indications for pancreatic stent in chronic pancreatitis?
Solitary narrowing / stricture in head or neck of pancreas with or without small solitary stone in the duct in the head / neck / body.
When does pancreatic stent fail in chronic pancreatitis?
Multiple strictures, multiple ductal stones, major disease in tail of pancreas, inflamed head with large stone load, very tight stricture. These are the situations where stenting is less likely to give lasting relief . It may give relief temporarily in some patients especially those who keep undergoing repeated stent exchange. However when the stent is removed they will more often than not get symptoms and finally come for surgery. This usually will happen 3- 4 years after 1st procedure.
What are the problems associated with stents?
Stent can get blocked, may dislodge / migrate / displace (move from its intended place), cause pain, cause infection or sometimes can perforate the pancreatic parenchyma while insertion.
What are the problems caused by stents to a patient undergoing surgery?
The most important problem is intra-abdominal infection after surgery from very resistant organisms which are very difficult to treat. Very few drugs are available for such infections & they are very expensive. It also leads to longer stay including ICU sometimes. It may need additional percutaneous drainage procedures. In short a patient who would otherwise go home in 5-6 days may need 15-20 days. Expenses will almost double. An unfortunate rare death also may occur if infection doesn’t come under control.
What are the advantages of timely surgery?
Surgery should always be done at the right time i.e. when the pancreatic duct is reasonably dilated. A too an early surgery can result in poor outcome. When o operated at right time before any stenting is done, patients recover faster and mostly without infections, are discharged sooner, expenses are less and outcome is better and long lasting when it comes to pain relief, digestion, diabetes and requirement of pancreatic enzymes.
Take home message for the reader
See a pancreas specialist surgeon before undergoing a pancreatic stenting, understand the role of stent versus surgery and then take the decision.
For Consultation Available At:
Timing: Monday To Friday - 9am To 5pm & Saturday 9am To 2pm
(Consultation Only by Appointment)
Address: Lilavati Hospital, A-791, Bandra Reclamation Rd, Bandra West, Mumbai, Maharashtra 400050
For Appointment call: 09821046391
Timing: Saturday 9am To 10am
(Consultation Only by Appointment)
Address: 93, ACI Hospital, 95, August Kranti Rd, Kemps Corner, Cumballa Hill, Mumbai, Maharashtra 400036
For Appointment call: 09821046391
Consultation Only by Appointment
Address: Raheja Rugnalaya Marg, Mahim West, Mahim, Mumbai, Maharashtra 400016